
Who’s Caring: University of Utah researchers are building bridges between home care and health care
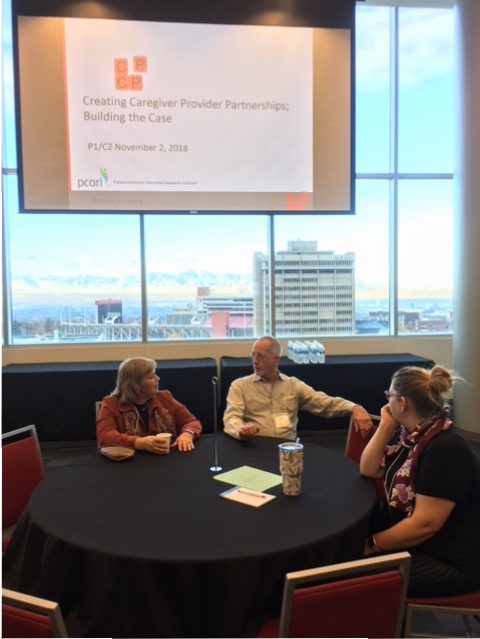
Recognizing the increasingly central role of family caregivers in navigating the economic and logistical healthcare challenges facing patients, professor Debra Scammon, Emma Eccles Jones Professor of Marketing and former director of the University of Utah’s Masters of Health Administration, along with colleague Christie North, recently hosted the second of four community engagement conferences at the David Eccles School of Business. Funded by the Patient Centered Outcomes Research Institute, the event brought together 13 family caregivers, five primary care providers, five patient and/or elder advocates, and eight researchers.
In collaboration with local and national partners, advisors, and organizations, Scammon and North are working to better understand the needs of the more than 330,000 family caregivers in Utah who provide roughly 300 million hours of unpaid work, which is valued at approximately $4.1 billion annually. Their work focuses on the perspective of family caregivers, healthcare providers, and care teams. Their aim is to better prepare both caregivers and provider teams for more productive partnerships.
Caregivers regularly assume a variety of roles and responsibilities, often with little training or experience. Their commitment and dedication in supporting the healthcare of loved ones can preserve autonomy and crucial social support networks. Further, home-based care can delay or prevent expensive, disruptive moves to assisted living facilities. The patient/caregiver dynamic has many advantages but also serious risks. Family caregivers may jeopardize their own physical, financial, and emotional well-being.
During their first two conferences, Scammon and North have identified resources and strategies that may increase caregivers’ support, knowledge, and stamina. Two key findings suggest that a caregiver’s early participation in decisions about a patient’s care, along with inclusion in that patient’s healthcare team, can improve their outlook and experience.
While the first conference prioritized a more thorough understanding of the family caregiver’s challenges and needs, the second conference focused on the healthcare provider’s experience with and barriers to caregiver engagement and inclusion.
To advance the goal of improved partnerships between family caregivers and healthcare providers, the second conference featured presentations by three providers with extensive experience of collaborative, team-based care, as well as family physician training. They are each experimenting with different ways to integrate the insights and experience of family caregivers into patients’ treatment and teams.
A representative from AARP’s Public Policy Institute discussed the significance of the Caregiver Advise, Record, and Enable (CARE) Act, initiated in Utah in 2016 and now adopted by 40+ states. It incorporates three activities — identifying a family caregiver, recording contact information in the patient medical record and alerting the caregiver to important decision making moments — thought to be essential in discharge planning for patients leaving the hospital. The requirements increase the probability of a family caregiver’s psychological and practical preparedness. The day concluded with a presentation from a family caregiver advocate providing examples of the many ways in which she has been able to support the cause of family caregivers.
Scammon and North have shared their work with policy groups locally with the Utah Commission on Aging, nationally with the American Society on Aging, and at academic conferences such as the Association for Marketing and Health Care Research. Scammon recently presented their work to the MHA students at the David Eccles School of Business, and MHA students have assisted with their conferences.







